You wake up, swing your legs out of bed, and there it is again – that familiar ache radiating across your lower back.
You’ve tried everything: heating pads, painkillers, different mattresses.
The question haunting you isn’t “how do I manage this today?” but rather, “can back pain be cured permanently, or am I stuck with this forever?”
Here’s the truth: For many people, back pain can be eliminated permanently through the right combination of treatments, lifestyle changes, and addressing root causes.

However, the answer depends heavily on what’s causing your back pain, how long you’ve had it, and your specific circumstances.
This isn’t the answer most articles give you, and that’s because the reality is more nuanced – and more hopeful – than a simple yes or no.
The Straight Answer: It Depends on These 3 Factors
Whether your back pain can be cured permanently comes down to three critical elements:
1. The underlying cause of your pain. Muscle strain responds differently than herniated discs, which respond differently than spinal stenosis.
According to the American Academy of Family Physicians, 60-90% of patients with acute lower back pain recover within six weeks, and 95% recover within 12 weeks with appropriate treatment.
2. How long you’ve had the pain. Acute back pain (lasting less than 6 weeks) has a much higher cure rate than chronic back pain (lasting more than 3 months).
3. Your commitment to evidence-based treatment. The combination of active treatment, lifestyle modification, and addressing underlying causes yields the highest success rates.
Let’s break down exactly what this means for you.
Understanding “Cure” vs “Management” (This Distinction Matters)
Before we go further, we need to clarify what “permanent cure” actually means in the context of back pain.
A true cure means: The pain is completely gone, the underlying issue is resolved, and it doesn’t return even without ongoing treatment. This is absolutely possible for many types of back pain.
Effective management means: The pain is controlled or eliminated through ongoing practices like exercise, posture awareness, or occasional treatment. You’re pain-free, but maintaining certain habits keeps it that way.
Here’s the good news: both outcomes mean you can live without back pain. The difference is mainly whether you need ongoing maintenance or not.
Types of Back Pain and Their Cure Potential
There are 3 main types of back pain:
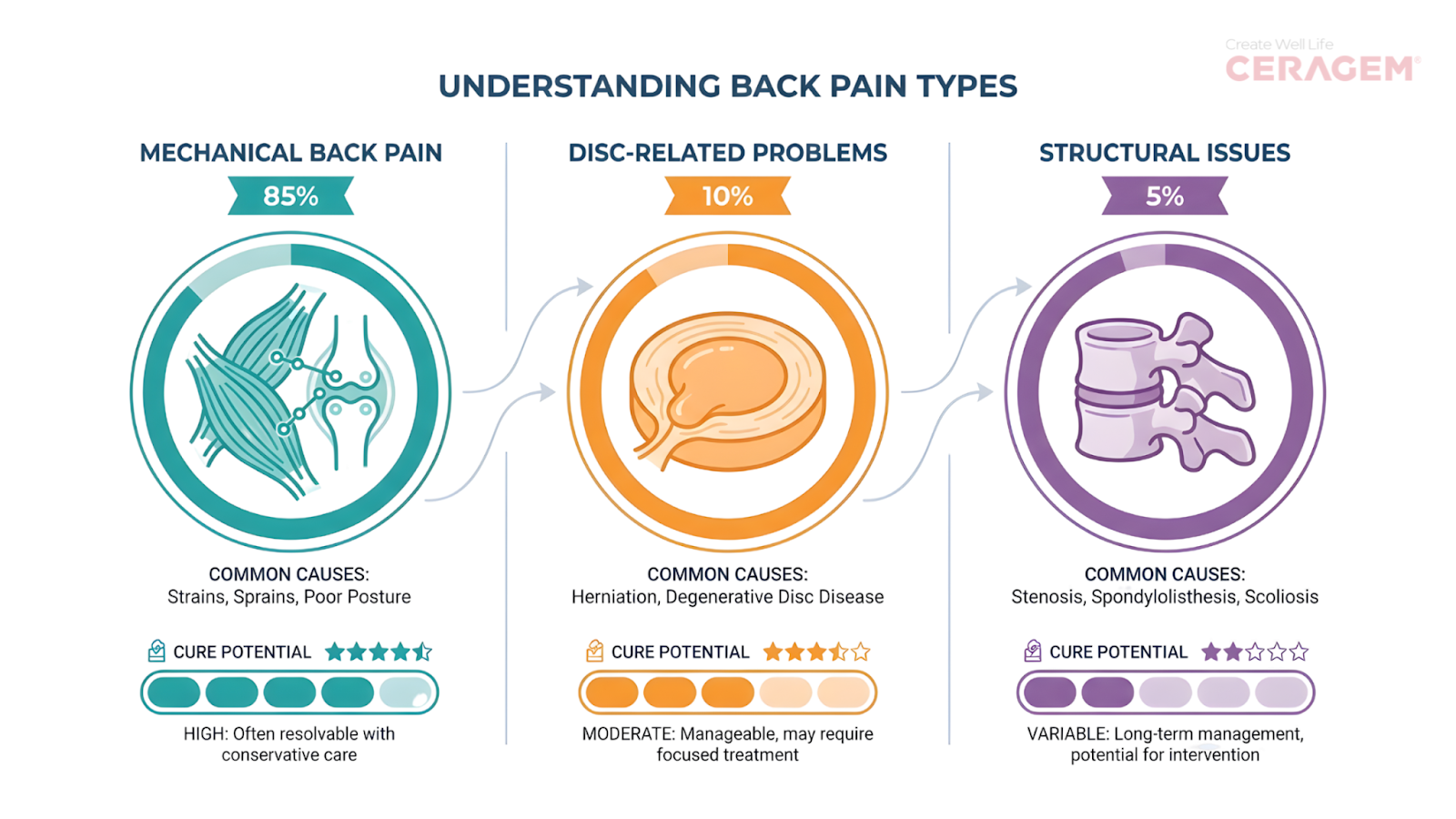
Mechanical Back Pain – High Cure Potential
This is caused by muscle strains, ligament sprains, poor posture, or muscular imbalances. It’s the most common type and also the most treatable.
Cure rate: With proper treatment including physical therapy and exercise, most people with mechanical back pain can achieve significant long-term relief.
According to a research published on PubMed Central, exercise and physical therapy are among the most effective treatments for mechanical low back pain.
Why it’s curable: The tissues heal naturally when given proper conditions, and correcting movement patterns prevents recurrence.
Disc-Related Problems – Moderate to High Cure Potential
This includes herniated discs, bulging discs, or degenerative disc disease.
Recovery rate: The good news is that many slipped or herniated discs improve without surgery. Research shows that the body can naturally shrink or absorb the slipped disc over time.
A major systematic review found that:
- About 96% of fully slipped (sequestrated) discs shrink on their own
- About 70% of extruded discs improve without surgery
- Bulges and protrusions also improve in many cases
Another recent meta-analysis found that overall, around 70% of lumbar disc herniations show natural resorption with conservative (non-surgical) treatment.
Why it often improves naturally: Your body has its own healing system. Special immune cells help break down and remove the slipped disc material through a process called phagocytosis. As swelling and nerve irritation reduce, pain gradually decreases.
Surgery vs non-surgery: A 2020 study published in the New England Journal of Medicine compared surgery with non-surgical treatment for long-lasting sciatica caused by a herniated disc.
The study showed that surgery gives faster pain relief, but many patients also improved with conservative treatment over time.
Structural Issues – Variable Cure Potential
This includes spinal stenosis, spondylolisthesis, severe arthritis, or spinal deformities.
Recovery rate: The outcome depends heavily on the severity of the condition. Some structural problems can be corrected with surgery, while others are managed long-term with physiotherapy, medication, lifestyle changes, or guided exercise. Improvement rates vary widely – some patients experience major relief, while others may need ongoing care.
For example, research on lumbar spinal stenosis suggests that surgery may provide faster symptom relief in some patients, especially in the short term.
However, long-term results between surgical and non-surgical treatment are often similar, and many people improve without surgery.
Evidence-Based Treatments That Actually Work for Permanent Relief
Let’s focus on treatments with strong scientific backing for achieving long-term or permanent relief.
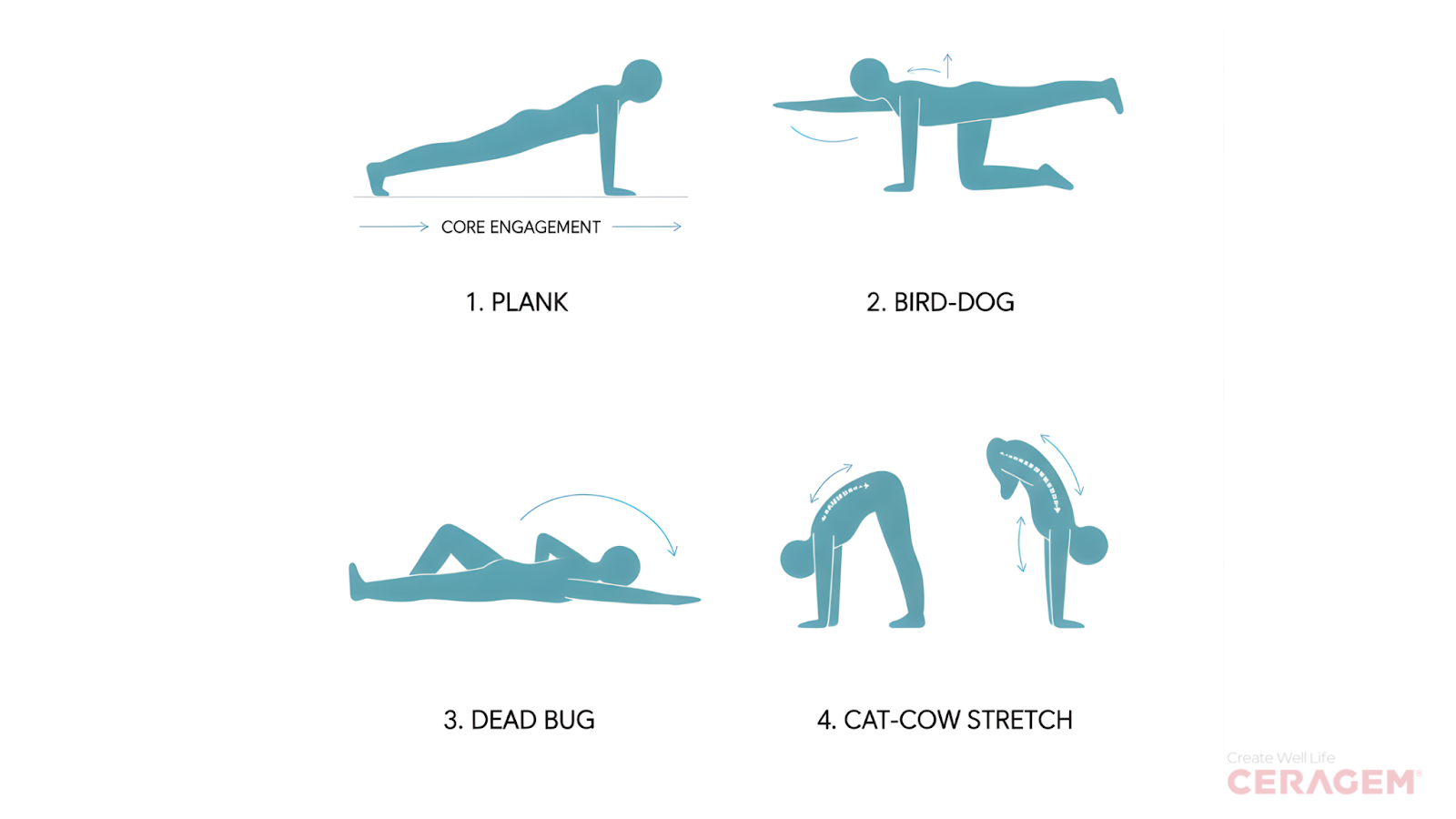
1. Physical Therapy and Targeted Exercise (Gold Standard)
Structured exercise therapy is widely recommended as a first-line treatment for chronic low back pain.
A large systematic review by the Cochrane Collaboration concluded that exercise therapy provides moderate-certainty evidence of clinically meaningful reductions in pain and improvements in function compared with no treatment or usual care (Hayden et al., 2021).
Why it works: Strengthens supporting muscles, improves flexibility, corrects movement patterns, and addresses root causes rather than just symptoms.
The protocol that works:
- Core strengthening (planks, bird dogs, dead bugs)
- Hip mobility exercises (hip flexor stretches, 90-90 stretches)
- Spine stabilization exercises
- Gradual progression over 8-12 weeks
- Continued maintenance exercises 2-3x weekly
2. Cognitive Behavioral Therapy (CBT) for Pain
Cognitive Behavioral Therapy (CBT) is a well-established psychological treatment for chronic pain. Rather than directly eliminating pain, CBT helps patients change unhelpful thought patterns, improve coping strategies, and increase daily functioning.
A major review published in American Psychologist concluded that CBT produces clinically meaningful reductions in pain intensity, pain-related distress, and disability, while also improving physical and emotional functioning in individuals with chronic pain (Ehde et al., 2014).
Why it works: Chronic pain involves changes in how your nervous system processes pain signals. CBT helps “retrain” your pain response and addresses the fear-avoidance cycle that perpetuates pain.
What it involves:
- Understanding the mind-body connection in pain
- Reducing fear of movement
- Breaking the pain-stress-tension cycle
- Developing coping strategies
Surprising fact: Psychological factors predict chronic pain development better than physical findings do. Addressing these can be the missing piece in achieving permanent relief.
3. Manual Therapy (When Combined with Exercise)
Manual therapy – such as spinal mobilization or manipulation – is often used alongside therapeutic exercise for chronic low back pain.
A recent meta-analysis published in Musculoskeletal Science and Practice (PROSPERO: CRD42023413778) found that adding manual therapy to exercise does not provide substantial additional short-term improvements in pain intensity compared with exercise alone.
However, the study did find that combining manual therapy with therapeutic exercise resulted in significant improvements in functional disability, both in the short term and long term.
Effective forms:
- Spinal manipulation (chiropractic or osteopathic)
- Massage therapy targeting specific muscle groups
- Myofascial release
- Dry needling for trigger points
The catch: Manual therapy alone rarely provides a permanent cure. It’s most effective as part of a comprehensive approach that includes strengthening and movement retraining.
4. Surgical Intervention (For Specific Cases)
Surgery is generally considered only for carefully selected patients with identifiable structural causes of back pain – such as disc herniation with nerve compression, spinal stenosis, or degenerative spondylolisthesis.
Large clinical trials, including the Spine Patient Outcomes Research Trial (SPORT), have shown that surgery can provide faster pain relief and functional improvement compared with non-operative care in appropriately selected patients with conditions such as lumbar disc herniation and spinal stenosis.
However, outcomes vary depending on diagnosis, patient selection, and surgical technique.
When Surgery May Be Considered
Surgery is typically reserved for cases involving:
- Severe nerve compression causing muscle weakness
- Loss of bowel or bladder control (a medical emergency, e.g., cauda equina syndrome)
- Progressive neurological deficits
- Structural instability (e.g., high-grade spondylolisthesis)
- Persistent, disabling symptoms after adequate conservative treatment (often 6–12 months, depending on the condition)
Important: Surgery Is Not Always a Cure
Research shows that a significant proportion of patients continue to experience pain after spine surgery – a condition often referred to as Failed Back Surgery Syndrome (FBSS).
The “Permanent Cure” Timeline: What to Realistically Expect
Understanding the healing timeline helps set realistic expectations and prevents discouragement.
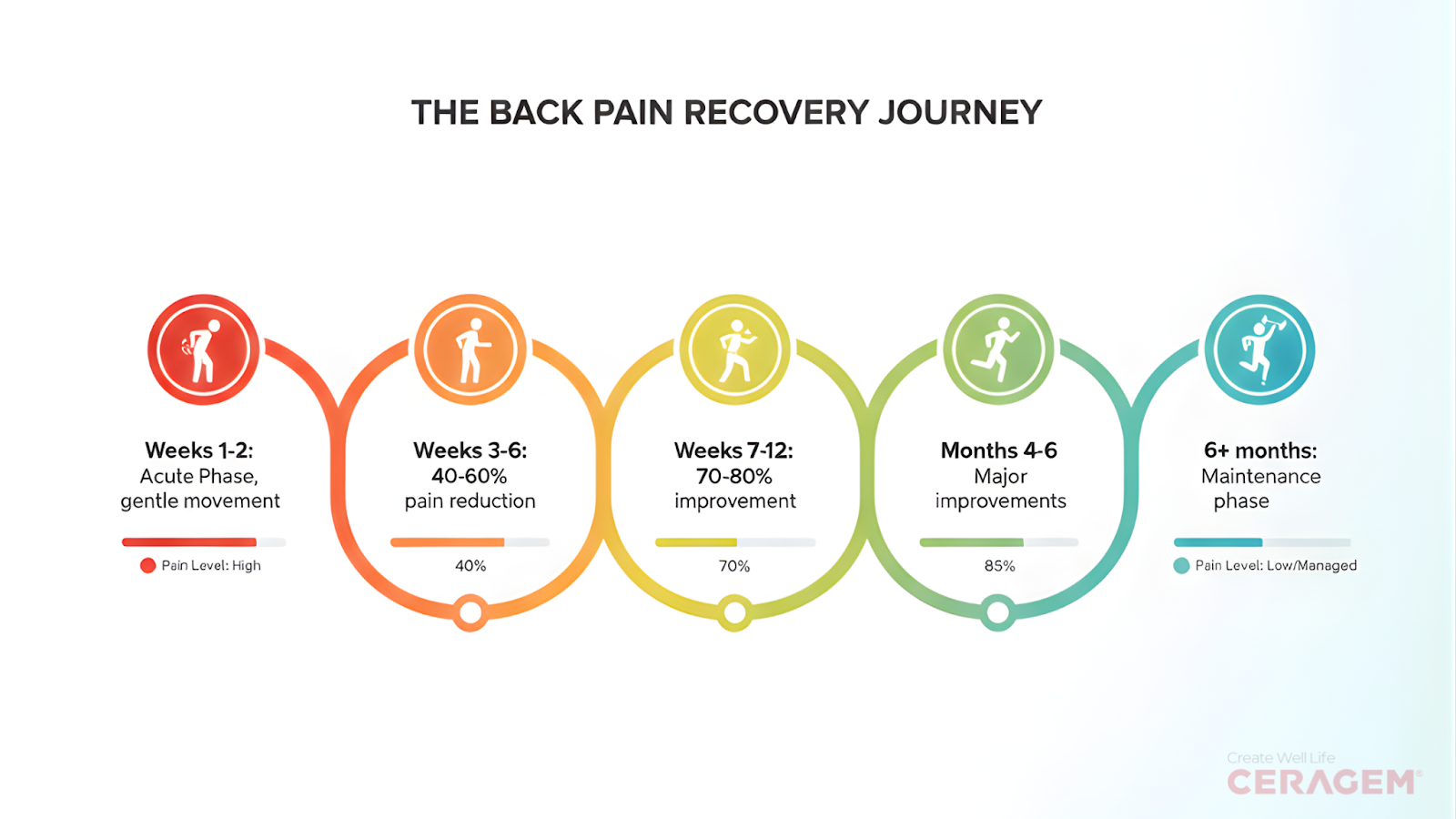
Weeks 1-2: Acute Phase
- Focus on pain reduction and gentle movement
- Avoid bed rest (worsens outcomes)
- Use ice/heat as needed
- Start gentle walking (10-15 minutes daily)
Weeks 3-6: Recovery Phase
- Begin structured exercise program
- Pain should reduce by 40-60%
- Increase activity gradually
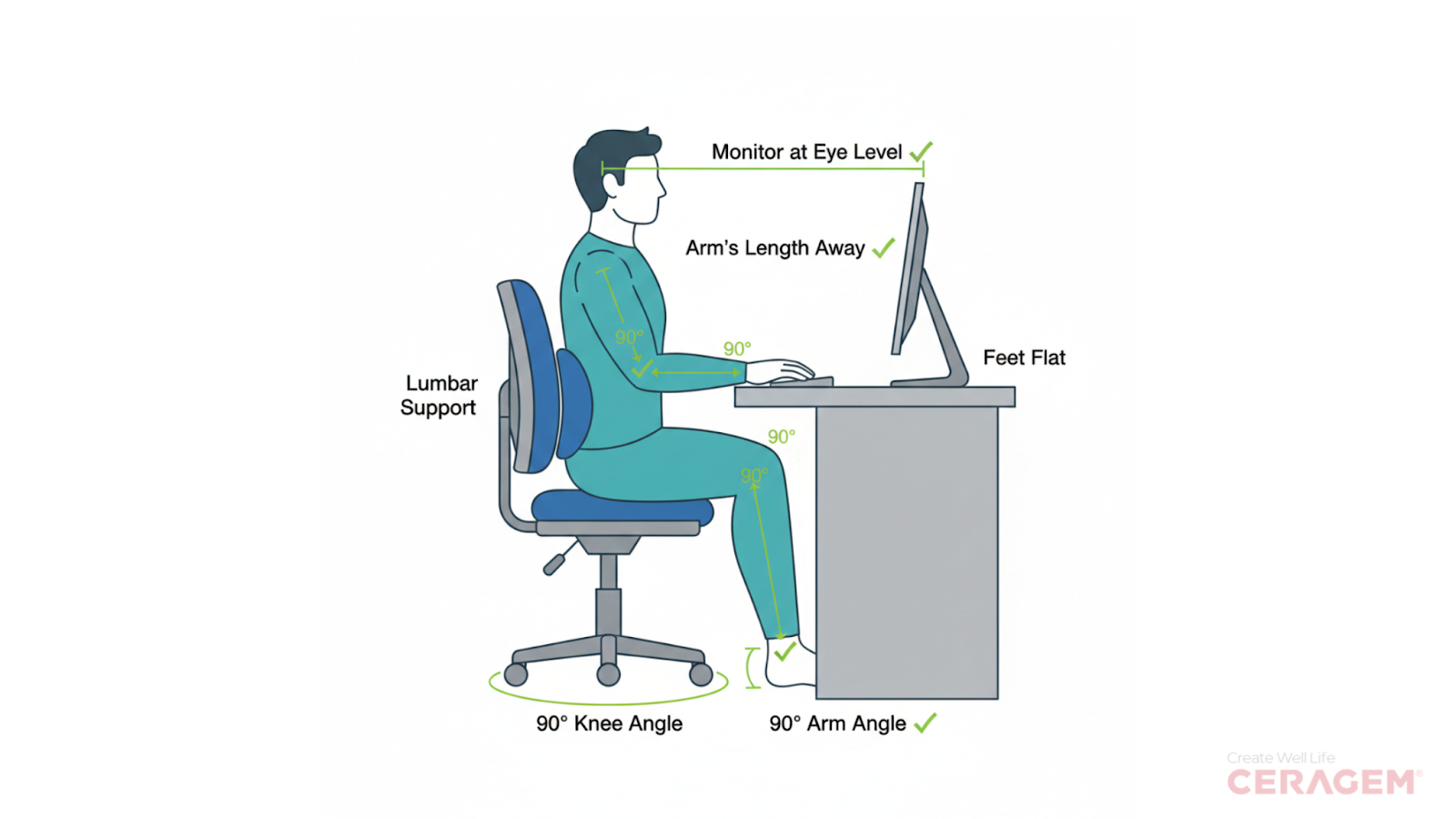
- Address posture and ergonomics
Weeks 7-12: Strengthening Phase
- Significant improvement in most cases (70-80% pain reduction)
- Build core and hip strength
- Return to normal activities with modifications
- Establish long-term exercise habits
Months 4-6: Consolidation Phase
- For chronic pain cases, this is where major improvements occur
- Full return to activities for most people
- Maintenance program established
Beyond 6 Months: Maintenance
- Keep up with 2-3x weekly exercise to prevent recurrence
- Monitor and adjust as needed
- Most people who reach this point stay pain-free long-term
The Lifestyle Factors That Make or Break Permanent Relief
Even the best treatment won’t provide a permanent cure if these foundational issues aren’t addressed.

1. Sedentary Lifestyle
Extended sitting has been associated with an increased risk of low back pain, particularly among office workers and individuals in sedentary occupations.
A review published in the European Spine Journal found that prolonged occupational sitting is linked to a higher likelihood of developing low back pain, although the exact level of risk varies across studies.
2. Poor Sleep Quality
Poor sleep increases pain sensitivity and slows the body’s natural healing processes. People with ongoing sleep disturbances are more likely to develop persistent musculoskeletal pain, including chronic back pain. Improving sleep quality can play an important role in long-term recovery.
3. Excess Weight
Excess body weight places additional mechanical stress on the spine, particularly the lower back. Over time, this added load can accelerate strain and degeneration.
Weight management is associated with improved pain levels and better functional outcomes.
4. Stress and Mental Health
Chronic stress can increase muscle tension, amplify pain perception, and prolong recovery.
Emotional factors such as anxiety, depression, and fear of movement are strongly linked to persistent back pain. Managing stress is an important part of long-term relief.
5. Smoking
Smoking reduces blood flow to spinal tissues and may accelerate disc degeneration, impairing healing.
Smokers are more likely to experience chronic back pain compared to non-smokers. Quitting smoking can support better spinal health and recovery.
Red Flags: When to Seek Immediate Medical Care
While most back pain is treatable without emergency care, certain symptoms require immediate attention:
- Loss of bowel or bladder control
- Progressive leg weakness
- Numbness in the groin or inner thighs (saddle anesthesia)
- Severe pain following trauma
- Unexplained weight loss with back pain
- Fever with back pain
- History of cancer with new back pain
These symptoms could indicate serious conditions like cauda equina syndrome, infection, or fracture that need urgent treatment.
Your Action Plan: 7 Steps to Pursue Permanent Relief
Based on current best evidence, here’s your roadmap to achieving lasting relief from back pain.
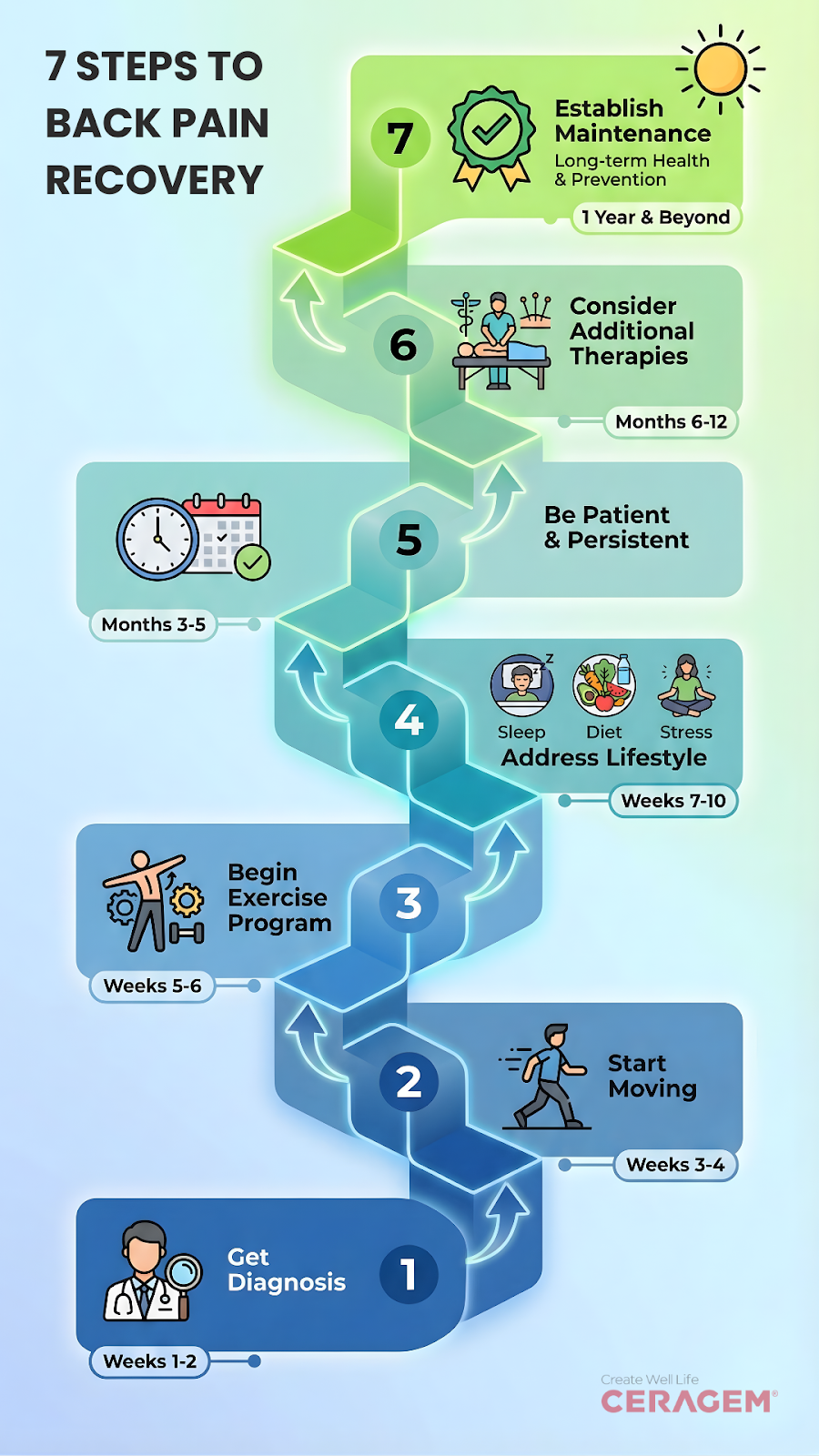
Step 1: Get an accurate diagnosis. See a healthcare provider (physician, physical therapist, or chiropractor) to identify the specific cause of your pain. Don’t rely on Dr. Google alone.
Step 2: Start moving immediately (unless contraindicated). Bed rest is your enemy. Even with acute pain, gentle walking and movement promote healing. Aim for 10-20 minutes of gentle activity daily.
Step 3: Begin a structured exercise program within 1-2 weeks. Work with a physical therapist to develop a personalized program. Research shows this is the single most effective treatment for long-term relief.
Step 4: Address lifestyle factors simultaneously. Improve sleep, reduce stress, optimize your workstation, manage weight if needed. These aren’t optional—they’re essential.
Step 5: Be patient but persistent. Most people see significant improvement by 6-12 weeks, but full resolution may take 3-6 months for chronic cases. Consistency beats intensity.
Step 6: Consider additional therapies if needed. If exercise alone isn’t enough after 6-8 weeks, add manual therapy, CBT, or consult about other options like injections or surgery.
Step 7: Establish a maintenance routine. Once pain-free, continue with 2-3x weekly exercise to prevent recurrence. This investment of 30-45 minutes weekly often makes the difference between cure and relapse.
The Bottom Line: Hope Backed by Science
Can back pain be cured permanently?
For the majority of people, yes – especially with early intervention and comprehensive treatment.
The key is shifting from passive treatments that merely mask symptoms to active approaches that address root causes. This means consistent exercise, lifestyle modifications, and patience through the healing process.
Your back pain may have different origins than someone else’s, and your path to recovery will be unique. But the science is clear: with the right approach, most people can achieve lasting relief and return to the activities they love.
The question isn’t whether a cure is possible – for most people, it is. The real question is: are you willing to invest the time and effort into the approaches that actually work?
If you’ve been suffering for weeks or months, take the first step today. Consult a healthcare provider, start moving gently, and commit to the process. Your future pain-free self will thank you.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before starting any treatment program. Individual results may vary, and some conditions require professional medical intervention.
Authors & Contributors
The Editorial Team at Ceragem India is a group of content professionals, researchers, and reviewers responsible for maintaining the quality and integrity of information published on the Ceragem India blog. Our focus is on delivering accurate, well-structured, and responsible content related to wellness, lifestyle, health awareness, and organizational initiatives.
Dr. Ashish Kumar Shrivastav is a Senior Consultant in Neurosurgery with over 34 years of professional experience in the field. He holds an MBBS (1986), MS in General Surgery (1990), and M.Ch in Neurosurgery (1994), and is recognized for his strong commitment to high-quality neurosurgical care.